Abstract
Introduction:
Bleeding risk is understudied in recently discharged medical patients and often less appreciated than venous thrombosis risk. Knowledge of both absolute and relative bleeding risk in people recently discharged from medical hospitalizations is needed to balance the risks of thrombosis and bleeding. We therefore quantified the relative and absolute risk of bleeding requiring hospitalization in patients recently discharged (up to 3 months) after a bleeding-free medical admission.
Methods:
We followed all primary care patients aged ≥18 at the University of Vermont Medical Center's primary care clinics from July 2010 to September 2019, capturing all hospitalizations and bleeding events that followed these hospitalizations for 3 months after discharge. Using International Classification of Disease (ICD) 9 and 10 discharge diagnoses, laboratory values, current procedure terminology (CPT) codes and flowsheet data for transfusion support, we developed and validated computable phenotypes to identify bleeding events. Validation was performed manually by abstracting 150 charts with bleeding events detected by the phenotype and 40 charts without a bleeding event. Present on admission (POA)-bleeding was defined if bleeding occurred <24 hours after admission, and hospital-acquired (HA) if it occurred ≥24 hours after admission. For this analysis, our outcome was POA-bleeding. Bleeding risk was estimated using successive 1-month intervals after discharge as a time-varying covariate in age- and sex-adjusted Cox proportional hazard models. The reference group was bleeding risk in people with no hospitalization in the prior 3 months. HA-bleeding occurring within 3 months of a previous hospitalization were not grouped with the prior hospitalization.
Results:
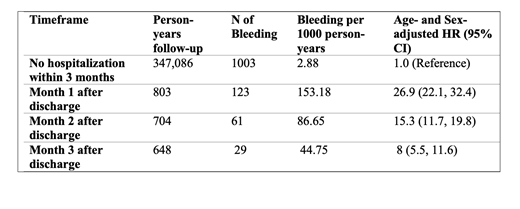
From 2010-2019, among 67,571 people with a mean age of 48 years (56.7% female) followed for a median of 6.2 years, there were a total of 14,266 medical hospitalizations and 1,784 hospitalized bleeding events (568 HA and 1216 POA). The bleeding computable phenotype had a positive predictive value of 79% and a negative predictive value of >99%. The rate of bleeding in people with no hospitalizations within the past 3 months was 2.88 per 1000 person-years. Over the 1 month after discharge, the rate was 153.8 per 1000 person-years decreasing to 61 per 1000 person-years in the second month after discharge and 29 per 1000 person-years in the third month after discharge. The age- and sex-adjusted HR for bleeding was 26.9 the first month after discharged and decreased respectively to 15.3 and 8 over successive 1-month intervals after discharge, relative to those with no hospitalization in the past 3 months (Table).
Conclusion:
In this northern Vermont population, the three months after a medical hospitalization was associated with dramatically increased risk of hospitalization for bleeding compared to people with no recent hospitalizations. Findings demonstrate how common bleeding is after hospitalization and emphasize on the need to develop methods to quantify bleeding risk.
Al-Samkari: Novartis: Consultancy; Moderna: Consultancy; Argenx: Consultancy; Rigel: Consultancy; Amgen: Research Funding; Dova/Sobi: Consultancy, Research Funding; Agios: Consultancy, Research Funding.